DR RACHAGAN : WHEN I HAD A STROKE …
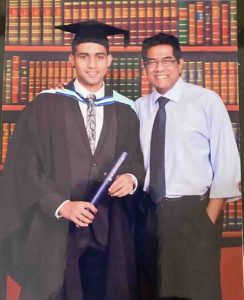
On June 1, 2009 – two years, two months and 13 days from the day of his stroke, Dr S.P. Rachagan, a consultant Obstetrician and Gynaecologist, returned to work at Subang Jaya Medical Centre (SJMC). Before he was able to do so, this doctor, a member of the Royal College of Obstetricians and Gynaecologists, UK, had to go through a stringent medical re-assessment process for a year. He tagged along with his peers, observed, assisted with procedures and kept a detailed log which, together with periodic assessments, were submitted to a special panel of medical experts set up by SJMC. After clocking in 26 years as an O&G consultant he describes this as a humbling experience.
Dr Rachagan suffered a haemorrhagic stroke on March 19, 2007. Three days earlier, on a Friday, he had gone for a coronary angioplasty procedure after it was confirmed that his artery on the left had narrowed by 95 percent. The next day he was discharged and as he had commitments, he remained busy. He didn’t stop to rest over the weekend and on Monday he went into work as usual. A thought that nags him to this day is: If I had rested after the procedure, would I have been spared the stroke?
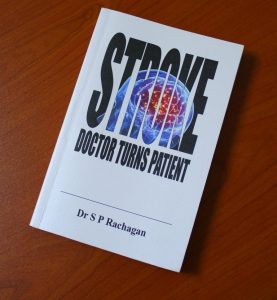
Here the doctor cum stroke survivor cum mentor and author of the book – STROKE: Doctor Turns Patient – shares his amazing recovery and how he is a living proof that after a stroke you can return to the community and even contribute effectively.

I had been working in SJMC since 1993. During my stroke I had tremendous support from my colleagues and friends in the hospital. So going back to the hospital two years later, in June 2009, was a wonderfully nice feeling. I was happy, excited and eager to go back to my old working grounds.
After going back to work, I continued my practice and officially retired seven years later, in August 2016. I was 57-years old when I had my stroke. I could have retired prior to my stroke. I did not want the decision to retire to be forced upon me by the stroke. I needed to take back control of my life; I did not want to allow the stroke to control my life.
Firstly, allow me to also share the one central point that was key to my recovery. During my first appointment with my speech therapist, she turned to me and asked: “Any questions, Dr Rachagan?”
The first thing out of my mouth was: “When can I get back to work?” I can imagine how totally out of place that question must have seemed to the therapist. To me, it was a natural question. As every single action or task that I did was focused on only one thing and that was getting well and returning to work. Focusing on the outcome – getting back to work – was crucial to my recovery. It is important for stroke patients to have clear goals, and these goals should act as incentives for us to work on our recovery.
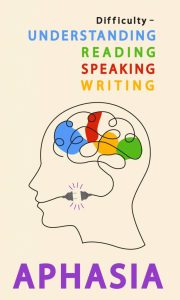
Coping with Aphasia
The most severe of all the deficits as a result of my left-brain haemorrhagic stroke was speech impairment, a condition known as aphasia. This was caused by the injury to the part of my brain containing language. The aphasia affected my four communication skills of speaking, listening, reading, and writing.
One weekend, my sister had come up from Singapore to see me. We were both seated at the dining table, when I suddenly turned to her and said: “I don’t know the name of this,” while pointing to the table, “or the name of this,” pointing to the chair!
It took my sister a few seconds to comprehend what I was saying. It was as if parts of my stock of vocabulary had been wiped out. My aphasia can be explained using the analogy of a library hit by an earthquake. The words were all there, but they were not on the shelves as they should have been. I had the mammoth task of correctly re-shelving all the books in my library. I had to place the words back into things and situations where they belonged.

One of the initial processes in addressing my aphasia was to work on vocabulary retrieval. I needed to take stock of my vocabulary. That was how I ended up with the ‘Peter and Jane’ book series. Yes, the children’s book published by Ladybird was where I started. Here was I, an O&G consultant, relegated to the level of a pre-schooler. The books had been used by my two nieces when they were learning to read and my family decided it would also help me. Every evening I was coached on re-learning to read. I told myself that if the Peter and Jane books could get me up and moving, so be it. I had no qualms about starting with them. Well, the saving grace was that I graduated from Peter and Jane within a month!
In addressing the challenges with aphasia, I sought professional support from Ms Cecilia Santiago, a speech therapist in Malaysia (who was with NASAM then but worked on this case within her private practice) and Dr Phua Sin Yong in Singapore. As I progressed with the vocabulary retrieval, my therapists moved me to the next stage, specific to the hospital environment and medical terminologies. These were termed high frequency words. Since I had been frequently exposed to these words in the past, I would recollect them quickly. These sessions progressed from vocabulary to writing full sentences and later moving on to comprehension and reports.
The speech therapy sessions were important, but on their own they were insufficient for me to make a full recovery. The much-needed additional help came from friends and family. A family friend, the late Ms R. Nathan, a retired teacher, came by daily, except weekends, from 9am to noon. She made me read and write in English. My sister, a teacher, would prepare a variety of other comprehension tasks, worksheets and reading materials. To facilitate my recollection of words, she would also make photocopies of instruments I would normally use in a hospital. These were pasted all over my bedroom and dining room walls. This technique helps with coaxing familiar words to come out from the deep recesses of the mind.
Pushing for better recovery
Apart from the major speech impairment, my stroke also created muscular weakness in my right arm and leg, impacting my mobility. As soon as I regained consciousness, I was referred to a physiotherapist. It is important for stoke patients to start with physiotherapy immediately as delays in moving the muscles would compound the weakness further. I started with passive exercises, where someone held my limbs and moved them, even while in the HDU ward.
Upon shifting to the normal ward, I had physiotherapy sessions for an hour each day. These sessions continued even after I was discharged from the hospital. Initially, it was tiring. I had to take frequent breaks but was advised to continue pushing myself. Good advice for all stroke patients. The continuous hard work paid off. Within a month, I was able to walk around the neighbourhood unaccompanied. Soon, I was walking about 5km a day.
By the third month of my stroke, as I regained my strength, my exercise regimen included a workout with a personal trainer at a gym. The exercises helped in the prevention of contractions and shortening of the muscles.

The stroke gave me, paresthesia, a muscular weakness in my right toes with a tingling sensation. I have a habit of walking around the house in slippers but with this condition, I frequently found that the slippers on my right foot would have dropped off without my knowledge. I developed the habit of often looking down to check if my slippers were still there. That simply emphasised the deficit but did not stop the problem with runaway slippers. I then started using sandals so that the back strap would serve to keep my sandal in place. And for the tingling sensation, I have simply learnt to live with it.
Another of my muscular deficits was dysphagia, difficulty with the process of eating, drinking, and swallowing. This is quite a common effect of stroke and is caused by a weakness to the side of the throat. With this weakness, swallowing too quickly may result in the food going down the wrong passage, leading to coughing and choking.
In the initial days after the stroke, I was advised to consume soft food and try to avoid food with bones. I was asked to take more vegetables to reduce the possibility of choking. Fortunately, I inherited my mother’s eating habits. She and I were frequently the last ones to leave the dinner table. I always took my time in chewing the food well before swallowing. This habit has served me well after the stroke.
Managing facial and other weaknesses
During my younger days, my sister and I studied classical music. Perhaps a more accurate account would be that I was made to sit with my sister whenever the music teacher came to teach her. What started off as compulsion developed into a passion. I enjoyed singing for family and friends. But as the stroke impacted the muscles on the right side of my face, singing or even whistling, was a challenge.
I remembered an exercise my father used to do as part of his morning exercise regime and started doing it daily. I would stand in front of the mirror and mouth the words ‘two eggs’ or ‘egg yolk’ or the alphabets ‘Q-X’. The stretching as I mouthed these words or alphabets helped to strengthen the facial muscles. I would do this exercise for about one minute each time and as often as possible, while looking out for any droop.

There was also injury to my parietal lobe, the part of the brain that figures out the messages received from the five senses. In my case, the sensory deficit was to my smell, taste, and sight. For most stroke patients, the sense of smell and taste returns to normal within a couple of months when the swelling in the brain subsides. In my case, even when the swelling subsided, my sense of smell was not fully restored. Fortunately, what I experienced was not a total loss of smell and taste but rather a reduced, almost muted, sense of smell and taste which is there till today.
The sensory deficit to my sight was more severe. A lay person assumes that our vision depends wholly on the health of our eyes. In reality, our vision depends on having both a healthy eye to receive visual information, and a healthy brain to interpret and process that information. The stroke had damaged part of the neural pathway from my eye to the brain, consequently impacting my right vision. I was diagnosed as having a right homonymous hemianopia.
My main concern was my central vision. This was crucial for a doctor diagnosing a patient, and I had lost part of my central vision. The first question I asked when I was diagnosed with hemianopia was whether my vision could be restored. I was told that the brain is known to partially rewire itself, as part of the healing process. I was also informed of Vision Restoration Therapy (VRT) which could help with the healing.
VRT is a computer-based treatment which uses repeated points of light flashed on a computer screen to stimulate the retina, especially at the border of the blind area of a patient’s visual field. The results of each session were recorded and analysed and the therapy adjusted to my progress. The therapy had marginal impact on my vision. After the therapy all of my left peripheral vision and all of my central vision was restored. However, the VRT had done almost nothing for my right peripheral vision. Initially I felt dejected that the VRT results had not improved my right peripheral vision. But I was happy that I had all my central vision, which was crucial for the proper examination of my patients. As a stroke survivor I have learned to celebrate the improvements, adjust to the deficits that persist, and work towards even more recovery.

Today, when someone asks, how do you keep yourself occupied. I reply: “I am a loafer.” The official definition of a loafer is a person who avoids work and spends time idly. I am that person. I now spend my time going on holidays (hopefully my holidays will resume soon with the commencement of the vaccination exercise), spending time with family and friends, and making time to support other stroke survivors.